Legal Do Not Resuscitate Order Form
When facing serious health challenges, one of the decisions that individuals and their families may consider involves whether or not to use life-sustaining measures in the event that the individual's heart stops or they stop breathing. This is where the Do Not Resuscitate (DNR) Order form becomes a crucial document. It serves as a directive to medical personnel, indicating the patient's wish to forgo certain life-extending procedures. Understanding the ins and outs of this form – from its legal standing across different states to the implications for patient care – is essential for making informed decisions that respect the individual’s wishes. This discussion will encompass the foundation of the DNR Order, including who can sign it, under what circumstances it can be invoked, and how it fits into the broader scope of medical and ethical considerations faced by patients, families, and healthcare providers alike. Amidst navigating these complex issues, the significance of clear communication and legal guidance cannot be overstressed, ensuring that the choices made are both informed and faithfully executed when the time comes.
State-specific Do Not Resuscitate Order Forms
Example - Do Not Resuscitate Order Form
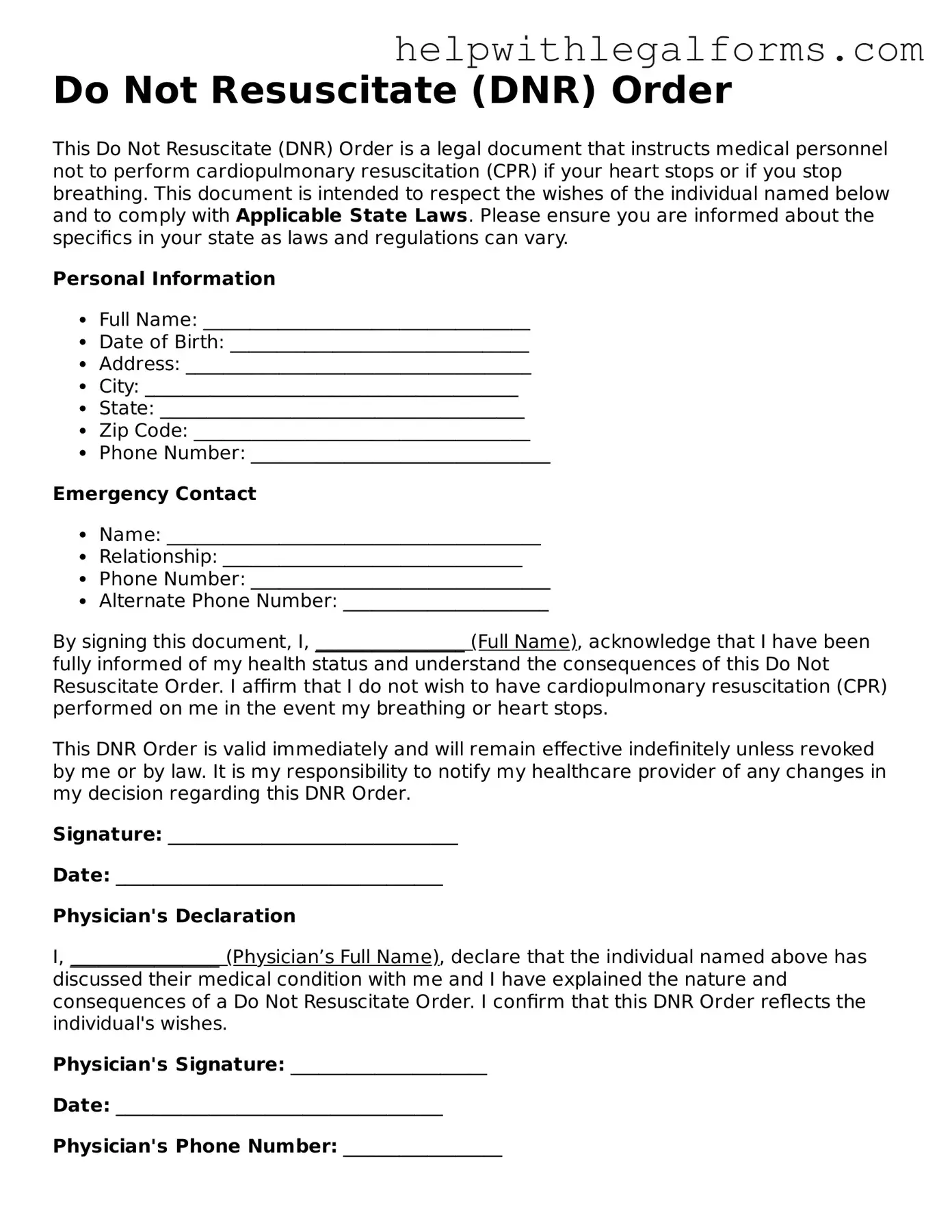
Do Not Resuscitate (DNR) Order
This Do Not Resuscitate (DNR) Order is a legal document that instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) if your heart stops or if you stop breathing. This document is intended to respect the wishes of the individual named below and to comply with Applicable State Laws. Please ensure you are informed about the specifics in your state as laws and regulations can vary.
Personal Information
- Full Name: ___________________________________
- Date of Birth: ________________________________
- Address: _____________________________________
- City: ________________________________________
- State: _______________________________________
- Zip Code: ____________________________________
- Phone Number: ________________________________
Emergency Contact
- Name: ________________________________________
- Relationship: ________________________________
- Phone Number: ________________________________
- Alternate Phone Number: ______________________
By signing this document, I, ________________ (Full Name), acknowledge that I have been fully informed of my health status and understand the consequences of this Do Not Resuscitate Order. I affirm that I do not wish to have cardiopulmonary resuscitation (CPR) performed on me in the event my breathing or heart stops.
This DNR Order is valid immediately and will remain effective indefinitely unless revoked by me or by law. It is my responsibility to notify my healthcare provider of any changes in my decision regarding this DNR Order.
Signature: _______________________________
Date: ___________________________________
Physician's Declaration
I, ________________ (Physician’s Full Name), declare that the individual named above has discussed their medical condition with me and I have explained the nature and consequences of a Do Not Resuscitate Order. I confirm that this DNR Order reflects the individual's wishes.
Physician's Signature: _____________________
Date: ___________________________________
Physician's Phone Number: _________________
Note: Please review and ensure compliance with the laws of your specific state regarding Do Not Resuscitate Orders. Some states may require notarization or additional documentation for this document to be considered legally valid.
PDF Form Attributes
| Fact Name | Description |
|---|---|
| Purpose | A Do Not Resuscitate (DNR) Order form instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) if a patient's breathing stops or if the patient's heart stops beating. |
| Creation | A DNR Order is usually created by the patient or their health care proxy in consultation with their doctor, based on the patient's medical condition and preferences regarding end-of-life care. |
| Legality | DNR Orders are legally binding in all U.S. states, but the form and requirements vary by state. |
| State-Specific Laws | In each state, specific statutes and regulations govern the creation, recognition, and implementation of DNR Orders. Patients must comply with their state's legal requirements to ensure their DNR Orders are valid. |
| Importance | Having a DNR Order in place ensures that a patient's medical treatment preferences are respected and followed, particularly in situations where they are unable to communicate their wishes directly to medical personnel. |
Instructions on How to Fill Out Do Not Resuscitate Order
A Do Not Resuscitate (DNR) Order is a legal document that informs medical personnel not to perform cardiopulmonary resuscitation (CPR) if a patient stops breathing or if the patient's heart stops beating. It is prepared in advance by a patient who decides not to have CPR performed or by a healthcare proxy acting according to the patient's wishes. Completing a DNR order is a significant step for an individual and involves careful consideration and, often, consultations with healthcare providers and family members. To ensure clarity and legal validity, it's crucial to fill out the form correctly. Here are the steps generally needed to complete a DNR order form properly.
- Review the entire form before writing anything. Read through the document to understand the information needed and ensure you have all the necessary details on hand.
- Provide the patient’s full name and date of birth. This information identifies the patient and should be written precisely as it appears on official identification.
- State the patient’s address and phone number. This is essential for contacting the patient or verifying their identity.
- Include the name and contact information of the patient’s healthcare proxy, if applicable. This person is authorized to make medical decisions on behalf of the patient.
- Detail any specific wishes regarding resuscitation. Some forms allow for nuances in the DNR order, such as conditions under which resuscitation efforts might be desired.
- Have the form signed by the required parties. In most jurisdictions, this includes the patient or their healthcare proxy and the attending physician. Ensure that you are aware of the specific signing requirements in your area, as they can differ.
- Date the form. The date is critical for establishing when the DNR order went into effect.
Once properly filled out and signed, the Do Not Resuscitate order communicates a patient's wishes regarding CPR and similar life-saving interventions. This document then becomes part of the patient's medical records. In the event of a medical emergency, healthcare providers will consult this document to guide their actions. It's important for patients and healthcare proxies to discuss this document with family members and to inform healthcare providers to ensure the patient's wishes are respected.
Crucial Points on This Form
What is a Do Not Resuscitate Order (DNR) form?
A Do Not Resuscitate Order, commonly referred to as a DNR form, is a legal document that instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) or other lifesaving measures if a person's breathing stops or if their heart stops beating. This is used for individuals who, due to a serious illness or frail condition, decide that they do not want such interventions. It is important to consult with a healthcare provider when considering a DNR to ensure it aligns with the individual's health status and wishes.
Who should consider a DNR Order?
Individuals who might consider a DNR order include those with a terminal illness, severe chronic health conditions, or those who wish to avoid aggressive medical interventions at the end of life. Such decisions are very personal and usually come after thoughtful discussions with family members, healthcare providers, and sometimes religious or spiritual advisors. Ultimately, it's for anyone who, in consultation with their healthcare professionals, decides that the quality of life would not be improved by aggressive interventions in the event of cardiac or respiratory failure.
How can someone set up a DNR Order?
To set up a DNR Order, the individual needs to discuss their wishes with their healthcare provider. The healthcare provider will then help them understand their options and the implications of a DNR order. If the person decides to proceed, the healthcare provider will typically prepare the necessary documentation, which must be signed by the patient (or their legally authorized representative if the patient is unable to do so) and often requires a witness or additional healthcare provider’s signature. This process ensures that the patient’s wishes are documented clearly and legally.
Is a DNR Order the same as a living will?
No, a DNR Order and a living will are not the same. While both documents relate to end-of-life care, a DNR is specifically a directive against CPR and certain life-sustaining treatments if a person stops breathing or their heart stops beating. A living will, on the other hand, is a broader document that outlines a person's wishes regarding a variety of medical treatments and interventions in the event they are unable to communicate their decisions due to a serious illness or incapacitation. People often have both documents as part of their advance directives.
Can a DNR Order be revoked or changed?
Yes, a DNR Order can be revoked or changed at any time by the person it concerns. The individual simply needs to inform their healthcare provider of their desire to revoke or amend the order. The healthcare provider will then document the change or revocation and ensure that the individual's medical records appropriately reflect their current wishes. It is crucial for individuals to communicate any change in their decisions regarding a DNR to all relevant parties, including family members and caregivers.
Does having a DNR Order affect the quality of other treatments?
No, having a DNR Order does not impact the quality of care a person receives for other medical conditions or emergencies. It specifically instructs healthcare providers not to initiate CPR or advanced life support techniques in the event of cardiac or respiratory arrest. It does not preclude the person from receiving other forms of medical care, treatments for pain, or any other healthcare services aimed at providing comfort and addressing other health concerns. The primary goal is to respect the individual’s wishes regarding end-of-life care while ensuring they receive the appropriate support and treatment for their condition.
Common mistakes
Filling out a Do Not Resuscitate (DNR) Order is a significant step in healthcare planning, directing medical personnel not to perform CPR if your heart stops or you stop breathing. Unfortunately, mistakes can happen during this process. Understanding and avoiding these common errors can ensure your wishes are accurately documented and followed.
-
Not discussing the decision with family or healthcare providers. Before completing a DNR form, it's crucial to talk about your decision with close family members and your primary healthcare provider. This discussion ensures everyone understands your wishes and can support them in an emergency.
-
Incorrect or incomplete information. Filling out any form requires attention to detail, but the accuracy on a DNR is crucial. Frequently, individuals might skip questions or fill in incorrect information about themselves or their healthcare proxy. It's essential to double-check each section to confirm all the information provided is correct and complete.
-
Not having the form properly signed or witnessed. A common oversight is failing to follow the signing requirements for a DNR order to be legally valid. Typically, this involves not only your signature but also signatures from witnesses or a notary, depending on state laws. Without these signatures, the DNR might not be recognized in a medical emergency.
-
Failing to inform key people of the DNR order. After completing and signing a DNR, a critical step that's often missed is informing relevant parties about its existence. This includes family members, healthcare proxies, and frequently your primary care doctor. For the DNR to be effective, it's necessary for first responders and medical personnel to be aware of and have access to your DNR order, should an emergency arise.
Being mindful of these mistakes when filling out a Do Not Resuscitate Order can help ensure that your healthcare wishes are honored. A carefully completed and managed DNR can provide peace of mind, knowing that your preferences are clear and will guide your medical care in times when you might not be able to communicate your desires directly.
Documents used along the form
Creating a comprehensive healthcare plan, especially for end-of-life care, involves more than just a Do Not Resuscitate (DNR) Order. A DNR form is critical for those who wish to forego CPR or other life-sustaining treatments during an emergency. However, to ensure your healthcare wishes are fully understood and respected, it's wise to consider other legal forms and documents that address various situations and aspects of care. Here's an overview of some key documents that are often used in conjunction with a DNR order:
- Living Will: A living will lays out your wishes for medical treatment and life-sustaining measures in the event that you’re unable to communicate them yourself. This can cover a range of treatments, not just resuscitation.
- Healthcare Power of Attorney (POA): This document designates someone you trust to make medical decisions on your behalf if you're incapacitated. This person is often referred to as a healthcare proxy or agent.
- Physician Orders for Life-Sustaining Treatment (POLST): A POLST form complements a DNR order by providing more comprehensive instructions about a range of life-sustaining treatments you do or don't want, beyond just CPR.
- Advance Directive: An advance directive can include both a living will and a medical POA, consolidating your wishes and delegations of authority into one document.
- Organ and Tissue Donation Form: This form records your decision to donate organs and tissues after death, which can be a separate document or part of your driver’s license or state ID process.
- Durable Power of Attorney for Finances: Although not directly related to your healthcare, this document is crucial for ensuring that your financial matters are handled by someone you trust if you become unable to manage them yourself.
- Guardianship Arrangement: If you have dependents, a guardianship arrangement document specifies who you want to care for them in the event of your incapacity or death.
- HIPAA Authorization Form: This document allows designated individuals to access your medical records and speak with healthcare providers, ensuring your health proxy has the information needed to make informed decisions.
- Last Will and Testament: This document outlines how you want your property and assets distributed after you die, and, similar to a guardianship arrangement, can specify care for children or pets.
Preparing these documents in advance is a thoughtful way to care for yourself and ease the burden on your loved ones during difficult times. Each plays a unique role in defining and respecting your healthcare and personal preferences, providing peace of mind to both you and your family. It’s advisable to discuss your wishes with healthcare providers and a legal professional to ensure your documents are properly executed and reflective of your desires.
Similar forms
- Living Will:
A Living Will, much like a Do Not Resuscitate (DNR) Order, is a legal document where individuals specify their wishes regarding medical treatment in scenarios where they are unable to communicate their decisions due to a severe health condition. Both documents guide healthcare professionals on how to proceed with medical care, especially regarding life-sustaining measures.
- Healthcare Power of Attorney (HCPOA):
Similar to a DNR, the Healthcare Power of Attorney designates a person to make healthcare decisions on behalf of the individual if they become incapacitated. While a DNR specifically addresses resuscitation wishes, a HCPOA covers a broader range of medical decisions.
- Advance Directive:
An Advance Directive encompasses aspects of both the Living Will and HCPOA, allowing individuals to outline their healthcare preferences and appoint a decision-maker. Like a DNR, it serves to communicate the patient’s desires regarding end-of-life care and other critical medical decisions.
- Medical Orders for Life-Sustaining Treatment (MOLST):
MOLST forms, similar to DNRs, provide specific instructions about certain medical treatments, including resuscitation. These are doctor's orders that translate a person’s wishes into official medical orders, applicable across various care settings.
- Do Not Intubate (DNI) Order:
A DNI Order is closely related to a DNR as it specifically instructs healthcare providers not to perform intubation for artificial breathing. Both a DNR and a DNI are critical in planning end-of-life care preferences.
- Physician Orders for Scope of Treatment (POST):
Similar to a DNR, a POST form is a doctor's order that outlines a patient’s preferences for end-of-life care, including resuscitation and other treatments. It is designed for individuals with serious illnesses or at the end of life.
- Emergency Medical Services (EMS) DNR:
An EMS DNR specifically instructs emergency personnel not to administer CPR or other resuscitative measures in the event of cardiac or respiratory arrest. It is a type of DNR that is specifically implemented in emergency situations outside of the hospital setting.
- Five Wishes Document:
Though more comprehensive, the Five Wishes document shares similarities with a DNR, as it addresses personal, spiritual, and medical wishes at the end of life. It includes a person’s desires regarding life-support treatment, making it an essential tool for medical and end-of-life planning.
Dos and Don'ts
When navigating the complexities of a Do Not Resuscitate (DNR) Order form, understanding the dos and don'ts can make a significant difference. These directives are pivotal in guiding healthcare professionals about your wishes regarding resuscitation efforts in critical moments. Below is a curated list to assist you through this process:
Dos:
Verify the form is the correct version for your state, as requirements can vary.
Talk to your healthcare provider to clearly understand the implications of a DNR order and how it aligns with your health goals.
Ensure that all information is legible and completed accurately to prevent any confusion during emergencies.
Have the form signed by the required parties, which typically include the patient (or authorized representative) and the physician.
Make multiple copies of the signed form, keeping the original in a well-known, easily accessible place, and provide copies to your family, close friends, and healthcare providers.
If you have a healthcare proxy or a medical power of attorney, discuss your DNR order with them to ensure your wishes are well-represented.
Wear a DNR bracelet if your state offers them, as this can immediately inform emergency medical personnel of your DNR status.
Review and update your DNR order periodically, especially after any major health changes or hospitalizations.
Consider consulting with a legal advisor to ensure your DNR order complements other parts of your healthcare planning, like living wills or advance directives.
Don'ts:
Don't fill out the form without having a thorough discussion with your doctor about what a DNR order means for your specific health situation.
Don't leave parts of the form blank, as incomplete information may lead to unwanted interventions or confusion during emergencies.
Don't forget to communicate your decision regarding the DNR order with family members and loved ones, to minimize distress and ensure your wishes are followed.
Don't neglect to consider state-specific requirements and forms, as they can significantly differ and affect the validity of your DNR order.
Don't assume all healthcare providers and facilities automatically know your DNR status; ensure it's clearly communicated and documents are readily available.
Don't overlook the need for witnesses or notarization if your state's law requires these for a valid DNR order.
Don't put the form in a safe deposit box or any other secure location that isn't easily accessible 24/7 to those who might need it.
Don't fail to review and revise your DNR order if your health condition or preferences change over time.
Don't ignore the emotional aspects of this decision, and consider seeking support from counselors or support groups to navigate any feelings or concerns.
Misconceptions
There are several common misconceptions about Do Not Resuscitate (DNR) Orders. Understanding these misconceptions is crucial for making informed healthcare decisions:
A DNR order affects all medical treatments - This is false. A DNR order specifically applies to cardiopulmonary resuscitation (CPR) if a person's breathing or heartbeat stops. It does not impact other treatments or care the person may receive.
Doctors decide if a patient needs a DNR order - Actually, the decision to have a DNR order is up to the patient or, in some cases, the patient's healthcare proxy or family. Doctors can provide advice, but the choice belongs to the patient or their representative.
A DNR order is permanent - A DNR order can be revoked or modified at any time by the patient or their legal representative. Patients should discuss any changes in their healthcare preferences with their doctor.
Hospitals automatically know about a patient’s DNR order - Patients or their representatives need to provide the hospital or medical staff with the DNR order. It’s important to have multiple copies and make the healthcare team aware of it.
A DNR order means giving up on life - Choosing a DNR order is a personal decision often made to avoid aggressive medical intervention. It is about the quality of life and respecting the patient's wishes, not giving up hope.
Only elderly patients can have a DNR order - Patients of any age can have a DNR order based on their health preferences and conditions. The decision is based on the individual’s health care goals and conditions, not age.
DNR orders are only for the hospital setting - DNR orders can apply in various settings, including at home, in hospices, and in hospitals. It’s important to ensure that the order is accessible and known to caregivers in all healthcare environments.
Having a DNR order means you can’t receive palliative care - This is incorrect. Patients with a DNR order are still eligible for palliative care. The focus is on providing comfort and alleviating pain, rather than attempting resuscitation.
Key takeaways
When considering the implication of a Do Not Resuscitate (DNR) Order, understanding its purpose, legal considerations, and how it functions within healthcare settings is crucial for individuals and their families. Here are several key takeaways about filling out and using the DNR order form:
- Understanding the Purpose: A DNR order is a legal document that tells healthcare providers not to perform CPR (cardiopulmonary resuscitation) if a patient's breathing stops or if the heart stops beating. It is important for those with terminal illnesses or severe health conditions, where CPR might prolong suffering or be unlikely to result in a meaningful recovery.
- Discuss with Healthcare Providers: Before completing a DNR order, it's critical to discuss your wishes with a healthcare provider, such as a doctor, who can give insights into the medical implications of such a decision. This conversation will help ensure that the DNR order reflects your genuine desires and health care objectives.
- State-specific Forms: DNR orders are subject to state regulations, meaning the form and its requirements can vary from one state to another. Always use the correct, state-specific DNR form to ensure it is legally valid.
- Informed Consent: The person filling out the DNR form must have the capacity to understand the consequences of the order and give informed consent. If the person is unable to do so, a legally designated healthcare proxy or guardian may be authorized to make this decision on their behalf.
- Accessibility of the DNR Order: Once completed, the DNR order should be easily accessible. It should be placed in a prominent location and available to healthcare providers in case of an emergency. Consider also informing close family members or caretakers where the document is stored.
- Review and Revise as Necessary: Life circumstances and health conditions can change. Therefore, it's advisable to regularly review your DNR order and discuss any potential changes with your healthcare provider. Amendments to the order may be made to reflect your current health condition and wishes.
- Understanding the Scope: Be aware that a DNR order specifically addresses CPR and does not affect other forms of medical intervention, such as pain relief, oxygen, or other necessary treatments to provide comfort. Make sure to discuss the scope of your DNR order with your healthcare provider to ensure your wishes are clearly understood and followed.
Making decisions about end-of-life care is profoundly personal and can be difficult. However, by taking these key steps and considerations into account, patients and their families can ensure that their wishes are respected and that they remain in control of their healthcare decisions.
Other Forms
Release of Liability - Permission slip that legally frees an individual or organization from future culpability.
Garage Rental Lease - Included in this agreement are specifics on rent amounts, due dates, security deposits, and any permissible activities within the garage space.
Selling Limited Edition Prints - Provides a clear and formal outline of an art sale transaction, ensuring all legal aspects are covered and agreed upon by both parties.