Blank Do Not Resuscitate Order Form for Maryland
Making decisions about end-of-life care can be challenging and emotional. In Maryland, one way to ensure that an individual's wishes regarding such care are respected is through the completion of a Do Not Resuscitate (DNR) Order form. This significant document plays a crucial role in healthcare planning, especially for patients with severe, life-limiting illnesses or those who wish to avoid aggressive life-saving measures. The form indicates to healthcare providers that, in the event of a cardiac or respiratory arrest, no attempts should be made to resuscitate the individual. It is a powerful tool that requires thoughtful consideration, discussion with healthcare professionals and loved ones, and a clear understanding of what it entails. The form must be signed by both the patient (or their legally authorized representative) and the physician, ensuring that it reflects the patient's true wishes and that they are well-informed about their condition and the implications of completing such an order. Moreover, the Maryland DNR Order form is recognized across various healthcare settings, from hospitals to nursing homes, making it a universally respected directive within the state's healthcare system.
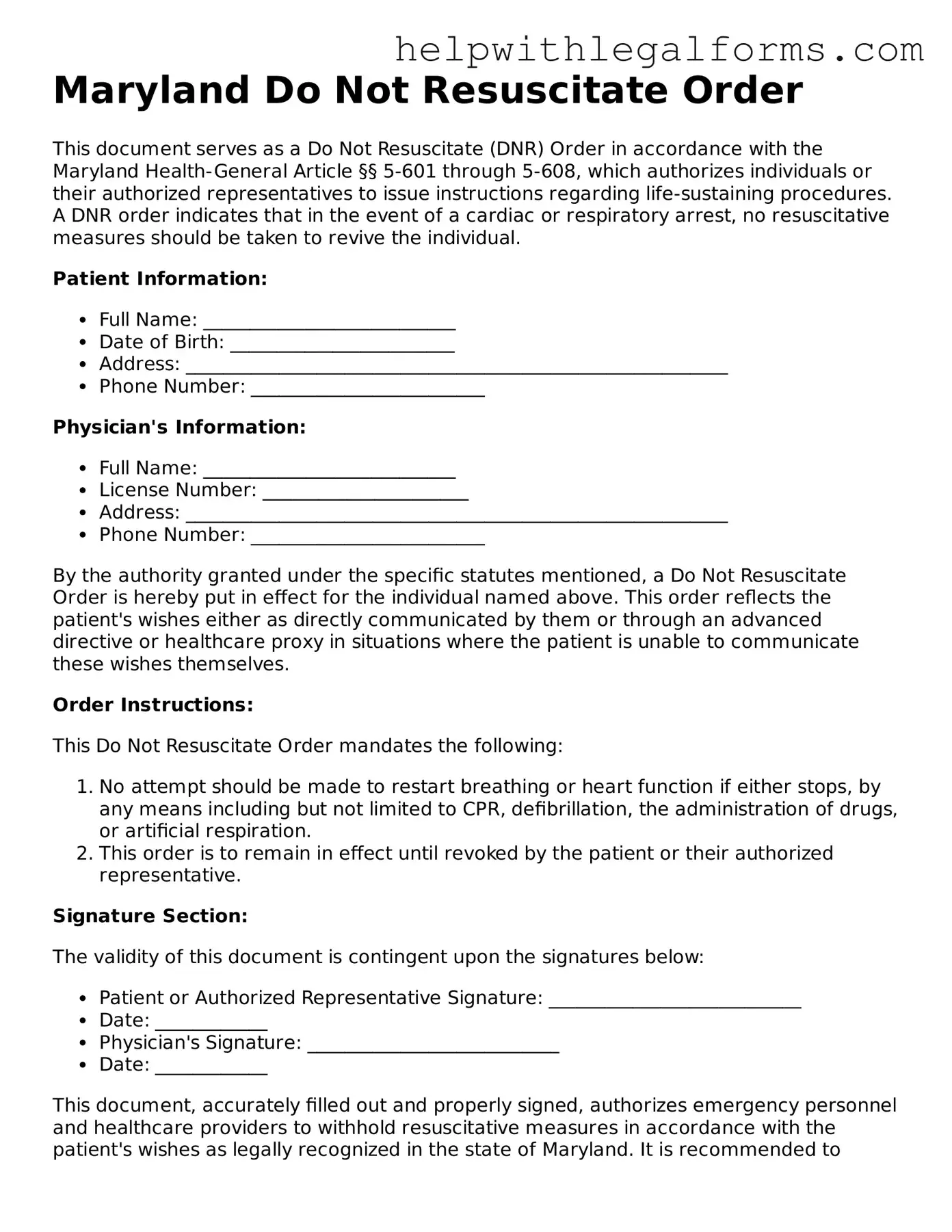
Example - Maryland Do Not Resuscitate Order Form
Maryland Do Not Resuscitate Order
This document serves as a Do Not Resuscitate (DNR) Order in accordance with the Maryland Health-General Article §§ 5-601 through 5-608, which authorizes individuals or their authorized representatives to issue instructions regarding life-sustaining procedures. A DNR order indicates that in the event of a cardiac or respiratory arrest, no resuscitative measures should be taken to revive the individual.
Patient Information:
- Full Name: ___________________________
- Date of Birth: ________________________
- Address: __________________________________________________________
- Phone Number: _________________________
Physician's Information:
- Full Name: ___________________________
- License Number: ______________________
- Address: __________________________________________________________
- Phone Number: _________________________
By the authority granted under the specific statutes mentioned, a Do Not Resuscitate Order is hereby put in effect for the individual named above. This order reflects the patient's wishes either as directly communicated by them or through an advanced directive or healthcare proxy in situations where the patient is unable to communicate these wishes themselves.
Order Instructions:
This Do Not Resuscitate Order mandates the following:
- No attempt should be made to restart breathing or heart function if either stops, by any means including but not limited to CPR, defibrillation, the administration of drugs, or artificial respiration.
- This order is to remain in effect until revoked by the patient or their authorized representative.
Signature Section:
The validity of this document is contingent upon the signatures below:
- Patient or Authorized Representative Signature: ___________________________
- Date: ____________
- Physician's Signature: ___________________________
- Date: ____________
This document, accurately filled out and properly signed, authorizes emergency personnel and healthcare providers to withhold resuscitative measures in accordance with the patient's wishes as legally recognized in the state of Maryland. It is recommended to discuss the implications of this order with a healthcare provider to ensure full understanding of its consequences.
PDF Form Attributes
| Fact Number | Detail |
|---|---|
| 1 | The Maryland Do Not Resuscitate (DNR) Order form is used to instruct medical personnel not to perform cardiopulmonary resuscitation (CPR) in the event a patient's breathing or heart stops. |
| 2 | This form must be signed by a licensed healthcare provider to be valid. |
| 3 | The form is part of Maryland's advance directives planning, as provided under Maryland Health-General Article, §§5-601 et seq. |
| 4 | Patients who wish to have a DNR order in place should discuss their wishes with their healthcare provider to ensure their desires are clearly documented and understood. |
| 5 | It is legally binding and must be followed by healthcare professionals, including EMS personnel, once properly executed. |
| 6 | The Maryland DNR form can be revoked by the patient at any time, provided they are competent to do so, by informing their healthcare provider verbally or in writing. |
| 7 | Having a DNR order in place does not impact the provision of other medical treatments, such as pain management or comfort care. |
| 8 | The form is available through the Maryland Department of Health and must be accurately completed to ensure its legitimacy. |
| 9 | Family members or healthcare agents may request a DNR order on behalf of an incapacitated patient, as long as it aligns with the patient’s known wishes or best interests. |
| 10 | A Maryland DNR order is state-specific and may not be recognized if a patient is transferred to a healthcare facility outside of Maryland. |
Instructions on How to Fill Out Maryland Do Not Resuscitate Order
Filling out a Maryland Do Not Resuscitate (DNR) Order is a significant step for those wishing to make clear their preferences regarding life-saving procedures. This document is designed to inform medical personnel about your decision to avoid resuscitative efforts in the event of a cardiac or respiratory arrest. It's a straightforward process but requires consideration and a careful approach to ensure your wishes are clearly communicated and legally documented.
Here's how to fill out the Maryland DNR Order form:
- Begin by gathering all required personal information, including your full name, date of birth, and address. This basic information helps identify you and ensures the DNR order is correctly attributed to your medical records.
- Contact your physician or healthcare provider to discuss your decision. They need to understand your wishes fully and agree that a DNR order is appropriate for your situation.
- With your healthcare provider, fill in the medical conditions section. This part requires a detailed description of your current health status and the medical conditions leading you to opt for a DNR order.
- Next, you and your healthcare provider must sign the form. Your signature indicates your informed decision and consent, while the healthcare provider's signature confirms they have discussed the DNR order with you and agree with your decision.
- Ensure the form includes the date of signing. The date is crucial as it shows when the DNR order became effective and can be important in situations where medical decisions need to be made swiftly.
- If applicable, have your healthcare proxy or legal guardian sign the form as well. This step is necessary if someone else is legally responsible for making healthcare decisions on your behalf.
- Finally, keep the completed DNR order in a location where it can quickly be found by family members or emergency responders. Copies should be given to your healthcare provider and any healthcare facilities where you receive care, such as a nursing home.
After completing and signing the DNR order form, take a moment to discuss your decision and the location of the order with close family members or friends. Ensuring those close to you are aware of your wishes and where to find your DNR order can alleviate confusion and stress in emergency situations. It's a compassionate step toward making sure your healthcare preferences are respected.
Crucial Points on This Form
What is a Do Not Resuscitate Order (DNR) form in Maryland?
A Do Not Resuscitate Order form in Maryland is a legal document that instructs medical personnel not to perform CPR (cardiopulmonary resuscitation) if a person's breathing stops or if their heart stops beating. It is used by individuals who do not wish to have these life-saving measures taken in the event of a medical emergency.
Who can request a DNR order in Maryland?
In Maryland, any competent adult can request a DNR order for themselves. A legal guardian or healthcare proxy can also request a DNR order on behalf of someone who is not able to make medical decisions for themselves.
How do I obtain a DNR order in Maryland?
To obtain a DNR order in Maryland, you must consult with your healthcare provider. The healthcare provider will discuss the implications and ensure you understand the decision. If you decide to proceed, the healthcare provider will prepare the DNR order and sign it.
Does the DNR order need to be notarized or witnessed in Maryland?
No, the DNR order in Maryland does not need to be notarized. However, it must be signed by your healthcare provider to be valid.
Where should I keep my DNR order?
Your DNR order should be easily accessible to emergency personnel. It’s recommended to keep it in a visible location, such as on your refrigerator, and to inform family members or housemates of its location. It's also wise to carry a copy with you or have an identification bracelet indicating you have a DNR order.
Can I change my mind after creating a DNR order in Maryland?
Yes, you can change your mind at any time. To cancel your DNR order, inform your healthcare provider, who can then help you rescind the order. It's also important to destroy any copies of the DNR order and notify anyone who was aware of its existence.
Is a DNR order the same as a living will?
No, a DNR order is not the same as a living will. A DNR order specifically addresses the use of CPR in emergency situations. A living will, on the other hand, provides more general instructions about a variety of medical treatments and interventions you do or do not want if you are unable to make decisions for yourself.
Does a Maryland DNR order work in other states?
While Maryland DNR orders are legally binding in Maryland, other states may have different regulations and requirements for recognizing DNR orders from out of state. It’s advisable to research and prepare according to the laws of any state you plan to visit or move to.
What happens if medical staff are not aware of my DNR order?
If medical staff are not aware of your DNR order, they may proceed with CPR or other life-saving measures in an emergency. This underscores the importance of making the DNR order readily available and communicated to your healthcare proxy, family members, and close friends.
Can a DNR order be included in medical alert systems or electronic medical records in Maryland?
Yes, a DNR order can be included in your electronic medical records or registered with medical alert systems. This helps ensure that the order is readily available to healthcare providers in emergency situations. Discuss this option with your healthcare provider.
Common mistakes
Filling out a Do Not Resuscitate (DNR) Order form in Maryland is a significant step that requires careful attention to detail. This document is essential for ensuring that a person’s wishes regarding resuscitation are respected during medical emergencies. Here are ten common mistakes people often make when completing this form:
Not discussing their wishes with a healthcare provider first. It's imperative to have a clear understanding of what a DNR order means and to ensure it aligns with your healthcare goals.
Failing to have the form signed by a physician. In Maryland, a DNR order must be signed by a licensed physician to be valid.
Leaving participant sections incomplete. Every field, including the patient’s name, date of birth, and other identifying information, needs to be filled out accurately.
Overlooking the need for witness signatures. Depending on the situation, a witness may be required to verify the authenticity of the patient's or healthcare proxy's signature.
Misunderstanding the scope of the DNR order. Some people mistakenly believe it applies to all medical treatments, but it specifically refers to not performing cardiopulmonary resuscitation (CPR).
Not specifying preferences regarding other life-sustaining treatments. While the DNR form focuses on CPR, it is important for individuals to communicate their wishes about other treatments through an Advance Directive.
Forgetting to share the completed form with their healthcare team and family. Once completed, the DNR form should be readily accessible to healthcare providers and loved ones.
Assuming the form is valid in all settings. A Maryland DNR order is generally recognized statewide, but policies can vary by institution, and it may not be automatically valid across state lines.
Not reviewing and updating the form periodically. Life circumstances and health care preferences can change, making it necessary to review and potentially revise the DNR order.
Overlooking digital storage options. In today’s digital age, storing a copy of the DNR order electronically can make it easily accessible to healthcare providers, especially in an emergency.
Remember: Filling out a DNR form is a personal and important decision. Making sure all aspects of the form are properly addressed can prevent misunderstandings during critical times. Always consult with healthcare professionals and loved ones when considering a DNR order.
Documents used along the form
When considering a Do Not Resuscitate (DNR) order in Maryland, several other forms and documents may be used in conjunction with it. These resources are designed to ensure a person's health care preferences are thoroughly documented and respected. Let's explore some of these essential documents.
- Advanced Directive: This document allows individuals to state their wishes regarding end-of-life medical treatment and appoint a health care agent. This person will make decisions for them if they become unable to do so themselves.
- Medical Orders for Life-Sustaining Treatment (MOLST): A MOLST echoes the wishes stated in an Advanced Directive, in a medically actionable form. Health care providers must follow these orders, which cover a wider range of treatments than DNR orders alone.
- Health Care Proxy: This document appoints another person to make medical decisions on someone’s behalf if they are not able to. It's a critical tool for ensuring that a person's medical treatment aligns with their values and preferences.
- Living Will: This specifies the types of medical treatments and life-sustaining measures an individual prefers or does not want in critical situations. Unlike a DNR, which is strictly about resuscitation, a Living Will can address treatments like feeding tubes or mechanical ventilation.
- HIPAA Authorization Form: This form allows health care providers to share an individual’s health information with designated persons. It can be crucial for family members or friends to gain access to information necessary to make informed decisions.
- Emergency Contact Form: Although not legally binding, this document provides health care professionals with contact information for an individual's chosen emergency contacts. It ensures that loved ones can be reached quickly in a crisis.
Together, these documents provide a comprehensive approach to planning for medical care. They help ensure that an individual's healthcare preferences are followed, even in situations where they cannot speak for themselves. By considering these forms alongside a Maryland DNR order, individuals can take a significant step toward controlling their medical treatment and end-of-life care.
Similar forms
Advance Directive (Living Will) - Much like the Do Not Resuscitate (DNR) order, an advance directive allows individuals to express their wishes regarding medical treatment should they become unable to communicate their decisions due to illness or incapacity. Both documents serve to guide healthcare professionals and loved ones in making medical decisions that align with the patient's preferences.
Power of Attorney for Health Care - This legal document designates an agent to make healthcare decisions on behalf of an individual, should they be unable to do so themselves. The DNR order and the power of attorney for health care are similar in that they both pertain to medical decision-making authority. However, a DNR specifically addresses the use of resuscitative measures, while a power of attorney can apply to a broader range of medical decisions.
POLST Form (Physician Orders for Life-Sustaining Treatment) - The POLST form is similar to a DNR in that it outlines a patient's preferences for end-of-life care, including the use of intubation, ventilators, and other life-sustaining treatments. Both are medical orders signed by a physician and are intended to ensure that a patient's wishes are respected during critical medical situations.
Medical Orders for Scope of Treatment (MOST) - Like the DNR, a MOST form is a doctor's order that clarifies which life-sustaining treatments a patient wants or does not want. It is comprehensive, covering more than just resuscitation, but it parallels the DNR in its objective to respect the patient's healthcare preferences at the end of life.
Healthcare Proxy - Also known as a medical power of attorney, a healthcare proxy appoints a person to make medical decisions on behalf of an individual if they become incapacitated. Similar to a DNR, it serves to ensure that medical treatment aligns with the individual's wishes. However, unlike a DNR, it delegates decision-making to another person, rather than specifying particular medical actions or non-actions.
Organ Donor Card - An organ donor card indicates an individual's wish to donate their organs and tissues after death. While its purpose differs from that of a DNR, both documents are crucial in medical contexts where they inform key decisions about a person's body after they are incapacitated or deceased, and ensure that these decisions are followed.
Five Wishes Document - The Five Wishes document goes beyond typical healthcare directives by addressing personal, emotional, and spiritual needs alongside medical wishes, similar to a DNR's role in articulating desires regarding life-sustaining treatment. It aims to cover a wider spectrum of patient concerns, making it a comprehensive planning tool.
Emergency Medical Information Form - This form contains important health information, such as allergies, medications, and medical conditions, much like a DNR contains critical information about a patient's wishes regarding CPR and resuscitation. Both forms are integral in emergencies to guide healthcare providers in delivering appropriate care.
Dos and Don'ts
When completing the Maryland Do Not Resuscitate (DNR) Order form, ensuring accuracy and compliance with state regulations is crucial. This document is sensitive and has significant implications. Below are recommended dos and don'ts to guide you through the process:
Do:
- Ensure that the patient or their legal healthcare decision-maker fully understands the implications of a DNR order before signing. The decision should be made after comprehensive discussions with a healthcare provider about the patient's medical condition and prognosis.
- Complete the form with accurate patient information including full name, date of birth, and other relevant personal details. This information is crucial for healthcare providers to identify the patient and understand their end-of-life wishes.
- Obtain the necessary signatures as required by Maryland state law. This typically includes the signature of the patient or their authorized healthcare decision-maker, and the attending physician or licensed healthcare provider authorized to sign the form.
- Keep the DNR Order easily accessible. Once the DNR form is completed and signed, it should be stored in a location where it can be quickly accessed by emergency personnel or healthcare providers in the event of a medical emergency.
Don't:
- Do not fill out the DNR form without consulting a healthcare provider. It is essential that the decision to enact a DNR order is made with a full understanding of the patient's medical condition and the specific implications of a DNR order.
- Do not leave sections of the form blank unless they are explicitly marked as optional. Incomplete forms may not be honored in an emergency, putting the patient at risk of receiving unwanted resuscitation efforts.
- Do not use guesswork when providing medical information or making healthcare decisions. If there is uncertainty, seek clarification from a healthcare professional to ensure that the form accurately reflects the patient's wishes and medical history.
- Do not forget to review and update the DNR order regularly. The patient's medical condition and preferences may change over time, so it is important to ensure that the DNR order remains accurate and reflects the current wishes of the patient or their healthcare decision-maker.
Misconceptions
The Maryland Do Not Resuscitate (DNR) Order form is an important document for many individuals and their families, but there are several misconceptions surrounding its purpose and implications. Clearing up these misunderstandings is key to ensuring that individuals can make informed decisions about their healthcare and end-of-life wishes.
- Misconception 1: A DNR order is only for the elderly or those with terminal illnesses.
Contrary to common belief, a DNR order can be appropriate for patients of any age. This includes individuals facing serious, life-limiting medical conditions where CPR would not offer a meaningful extension of life or would go against their values and wishes.
- Misconception 2: Signing a DNR means giving up on all types of medical treatment.
This is not the case. A DNR order specifically addresses the use of CPR (cardiopulmonary resuscitation) in the event of cardiac or respiratory arrest. It does not decline other forms of medical intervention or treatments that could provide comfort or address specific medical issues.
- Misconception 3: Only a patient can request a DNR order.
While it's true that competent individuals can request a DNR order for themselves, in instances where a patient is unable to make their own healthcare decisions, a legally authorized representative, such as a healthcare proxy or a family member, may also request a DNR order based on previously expressed wishes of the patient or best interests considerations.
- Misconception 4: A DNR order is irreversible.
A DNR order is not set in stone. It can be revoked or modified at any time by the patient or their legally authorized representative, ensuring that it reflects the current wishes of the individual concerning CPR.
- Misconception 5: DNR orders are effective everywhere.
DNR orders are state-specific and primarily effective within hospital settings or in the presence of emergency medical personnel. They might not be recognized in other states without a separate process or documentation, and they do not automatically apply to situations outside of healthcare facilities unless specifically noted (e.g., Maryland MOLST form for out-of-hospital situations).
- Misconception 6: A DNR order is the same as a living will.
While both documents relate to end-of-life decisions, they serve different purposes. A living will generally provides broader instructions about a person’s healthcare preferences, including but not limited to resuscitation. A DNR order specifically addresses the use of CPR.
- Misconception 7: Health care providers will consult family members before honoring a DNR.
Healthcare providers are legally required to follow a valid DNR order, regardless of the opinions or desires of family members at the time of an emergency. This highlights the importance of discussing one's wishes with family and healthcare providers in advance.
Understanding these misconceptions and the realities of a Maryland Do Not Resuscitate Order can empower individuals and families to make informed decisions that align with their values, beliefs, and medical preferences.
Key takeaways
Understanding and using the Maryland Do Not Resuscitate (DNR) Order form correctly is crucial for ensuring that a patient's wishes regarding resuscitation in emergency situations are honored. The following takeaways provide key insights into the process of completing and utilizing the DNR form in Maryland:
- Patients must voluntarily request a DNR order; it cannot be imposed upon them by others. The decision should be made by the patient, in consultation with their healthcare provider, after a thorough discussion of what the DNR entails.
- The DNR order must be signed by both the patient (or their authorized representative if the patient is unable to sign) and the patient's attending physician. The physician's signature indicates their agreement and the medical validity of the DNR order.
- A valid DNR order should be clearly displayed or easily accessible to ensure it is found by emergency personnel when they arrive. There are specific items, like bracelets or wallet cards, recognized by emergency medical services (EMS).
- A DNR order is applicable in various healthcare settings, including hospitals, nursing homes, and in the patient's home. Each setting may have specific procedures for recognizing and implementing DNR orders.
- Patients have the right to revoke their DNR order at any time. This decision must be communicated to their healthcare provider as soon as possible, to update their medical records and treatment plans accordingly.
- A DNR order does not mean that the patient will be denied other forms of medical care. It specifically addresses the use of CPR (cardiopulmonary resuscitation) and other resuscitative measures in the event of cardiac or respiratory arrest.
- Discussions about a DNR order should also explore other advance directives, such as living wills and healthcare power of attorney, which can provide comprehensive guidance on a patient's wishes for various medical situations beyond resuscitation.
- Physicians and healthcare providers have a responsibility to ensure that patients and their families understand the implications of a DNR order. This includes the potential outcomes and the nature of the care that will or will not be provided.
- Emergency medical personnel are legally bound to follow a valid DNR order. However, in the absence of a clear and accessible DNR order, they are required to perform resuscitation efforts.
- The Maryland Advance Directive form may include a DNR order as part of a broader document that addresses a variety of healthcare preferences and instructions. It's important to have all relevant documents properly filled out and in place to ensure one's wishes are known and respected.
Properly understanding and implementing a DNR order can significantly impact the respect of patient autonomy and the quality of care at the end of life. Legal and healthcare professionals play a key role in guiding patients and their families through this sensitive and important process.
Create Other Do Not Resuscitate Order Forms for US States
Georgia Do Not Resuscitate Form - While the decision for a Do Not Resuscitate Order can be complex, it often comes after thoughtful discussion with loved ones and healthcare providers.
Dnr Order - It is also an important piece for legal and ethical considerations in medical practice, respecting patient autonomy.