Blank Do Not Resuscitate Order Form for New Jersey
In New Jersey, individuals seeking to assert control over end-of-life medical decisions have the option to complete a Do Not Resuscitate (DNR) Order form. This document plays a crucial role in healthcare, particularly in situations where a patient's condition leads to cardiac or respiratory arrest. By completing a DNR form, a person explicitly indicates their wish not to have cardiopulmonary resuscitation (CPR) in the event that their breathing or heartbeat stops. Such an order is a testament to a patient's autonomy over their body and medical treatments at the most critical times. The form must be properly completed and signed by both the individual (or their legally authorized healthcare proxy) and the attending physician. This ensures that the healthcare team is legally bound to honor the patient's wishes. The DNR order is particularly relevant for patients with terminal illnesses or those who are in an advanced state of decline, where the chances of recovery from resuscitative efforts are minimal and the quality of life is a primary concern. New Jersey's approach to DNR orders underscores the state's commitment to respecting patient autonomy while navigating the complex interplay between medical ethics, patient rights, and the responsibilities of healthcare providers.
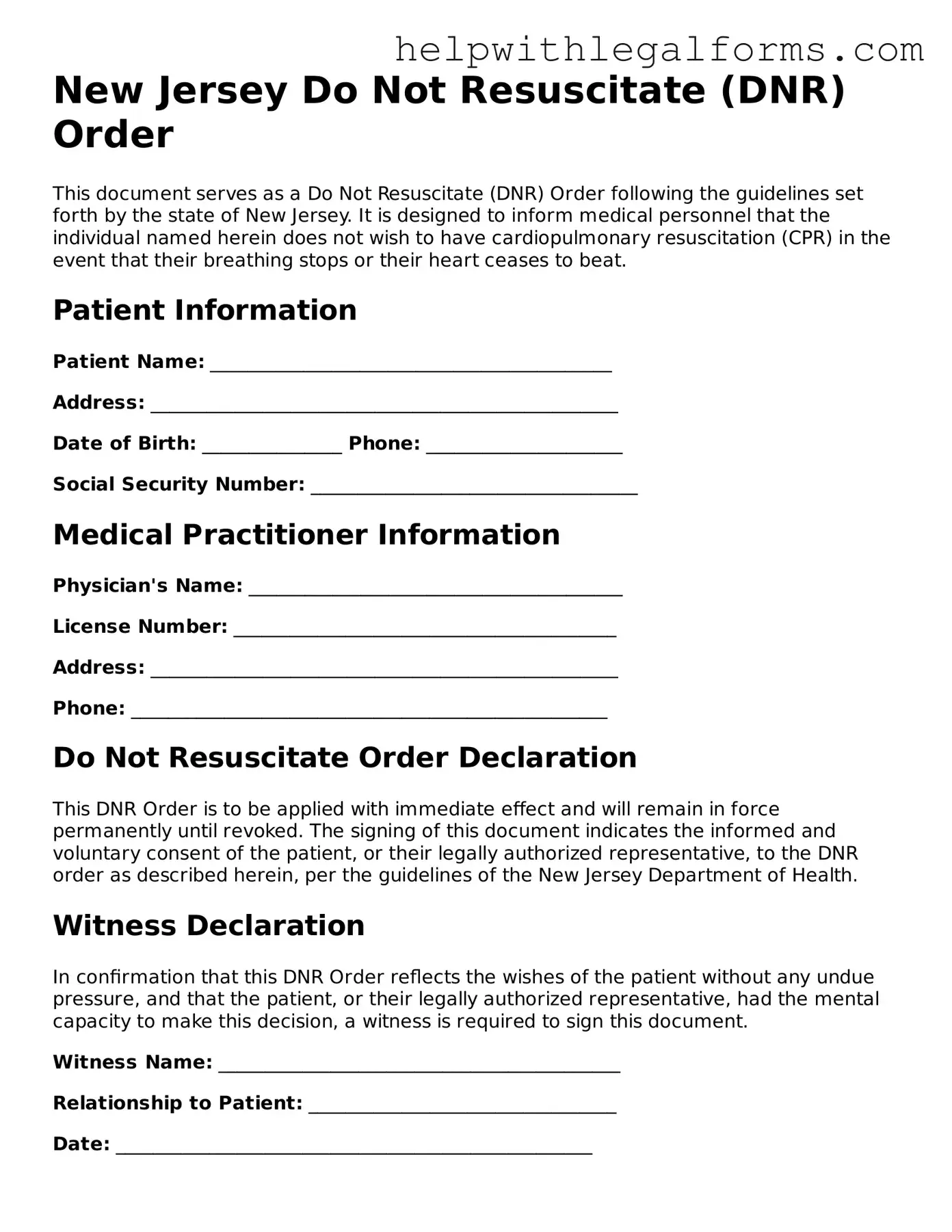
Example - New Jersey Do Not Resuscitate Order Form
New Jersey Do Not Resuscitate (DNR) Order
This document serves as a Do Not Resuscitate (DNR) Order following the guidelines set forth by the state of New Jersey. It is designed to inform medical personnel that the individual named herein does not wish to have cardiopulmonary resuscitation (CPR) in the event that their breathing stops or their heart ceases to beat.
Patient Information
Patient Name: ___________________________________________
Address: __________________________________________________
Date of Birth: _______________ Phone: _____________________
Social Security Number: ___________________________________
Medical Practitioner Information
Physician's Name: ________________________________________
License Number: _________________________________________
Address: __________________________________________________
Phone: ___________________________________________________
Do Not Resuscitate Order Declaration
This DNR Order is to be applied with immediate effect and will remain in force permanently until revoked. The signing of this document indicates the informed and voluntary consent of the patient, or their legally authorized representative, to the DNR order as described herein, per the guidelines of the New Jersey Department of Health.
Witness Declaration
In confirmation that this DNR Order reflects the wishes of the patient without any undue pressure, and that the patient, or their legally authorized representative, had the mental capacity to make this decision, a witness is required to sign this document.
Witness Name: ___________________________________________
Relationship to Patient: _________________________________
Date: ___________________________________________________
Signature
Patient or Legally Authorized Representative: ___________________________________________
Date: ___________________________________________________
Physician's Signature: ___________________________________________
Date: ___________________________________________________
Completion of this form adheres to the provisions of New Jersey law concerning DNR orders. It is recommended to keep this document easily accessible and to inform family members, caregivers, and healthcare providers of its existence and location.
Instructions for Revocation
To revoke this DNR Order, the patient or their legally authorized representative must inform the attending physician or healthcare provider verbally or through written communication. It is advisable to also destroy physical copies of the DNR Order to prevent unintentional use.
PDF Form Attributes
| Fact Name | Description |
|---|---|
| Purpose | Specifies a patient's wish not to receive cardiopulmonary resuscitation (CPR) in case they experience cardiac or respiratory arrest. |
| Governing Law | Guided by New Jersey's "Practitioner Orders for Life-Sustaining Treatment" Act (POLST) and related regulations. |
| Who Can Sign | The form can be signed by the patient (if capable), or their legally authorized health care representative. |
| Witness Requirement | Requires the signature of a witness, who verifies the identity of the signer and their voluntary execution of the form. |
| Effectiveness | Once signed, it is effective immediately and must be followed by health care providers. |
| Revocation | The patient or their authorized representative can revoke the order at any time through various forms of communication. |
| Accessibility | It must be readily accessible to health care providers and presented upon request to ensure its directives are followed. |
Instructions on How to Fill Out New Jersey Do Not Resuscitate Order
When someone is facing a terminal illness or is in a state of health where they do not want extraordinary measures taken to extend their life in the event of a cardiac or respiratory arrest, a Do Not Resuscitate (DNR) order can be an important tool. In New Jersey, filling out a DNR order involves detailing your wishes regarding resuscitation, signifying that in cases of severe medical emergencies, you prefer not to have CPR or other life-prolonging interventions performed on you. This document ensures that your healthcare preferences are known and honored by healthcare professionals. Given the gravity and significance of a DNR order, it's vital to complete the form accurately and thoroughly.
To properly fill out the New Jersey Do Not Resuscitate Order form, follow these steps:
- Begin by entering the patient's full name, including first, middle, and last names, to ensure there is no ambiguity regarding whose wishes are documented.
- Provide the patient's date of birth in the format MM/DD/YYYY. This helps healthcare providers verify the identity of the patient.
- Include the patient's full address, taking care to spell out street names and city names accurately. This information might be used in a health emergency to provide context or communicate with next of kin.
- Fill in the primary diagnosis. This is crucial as it provides the medical reason behind the DNR order, helping healthcare professionals understand the patient’s health status and decision.
- Specify any secondary diagnoses that are relevant to the patient's overall health condition or that could impact medical decisions during an emergency.
- List any allergies the patient has, especially to medications. This information can be lifesaving even in a situation where resuscitation is not performed.
- Detail the specific orders given by the physician regarding the DNR. This could include instructions on whether certain interventions like intubation, mechanical ventilation, or IV medications are allowed or prohibited.
- The physician’s name, license number, and contact information should be entered clearly. This information is necessary for the form’s validity and might be needed if there are questions regarding the DNR order.
- Both the patient (or their legally authorized representative) and the physician must sign the form. Ensure that these signatures are dated to confirm when the order was made effective.
After the form has been filled out, it is important to inform family members and any caregivers of its existence and location. The DNR order should be kept in a place where it can be easily found in an emergency, such as with other important medical documents or given to a healthcare proxy who has been legally designated to make medical decisions for the patient. In New Jersey, it is also advisable to review the DNR order periodically and after any significant changes in health status. This ensures that the document reflects your most current healthcare preferences.
Crucial Points on This Form
What is a Do Not Resuscitate Order in New Jersey?
A Do Not Resuscitate (DNR) Order in New Jersey is a medical directive to healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a patient's breathing stops or if the patient's heart stops beating. This order is used by individuals who wish to avoid potentially life-extending but possibly invasive medical interventions at the end of life. It is typically part of a broader approach to end-of-life planning.
How can one obtain a Do Not Resuscitate Order in New Jersey?
To obtain a Do Not Resuscitate Order in New Jersey, a patient must consult with their physician. The process involves a discussion about the patient's health status, the likely outcome of CPR, and the patient's wishes regarding end-of-life care. The physician then completes the DNR form, which must be signed by the physician and, ideally, by the patient or the patient’s legally appointed health care proxy if the patient is unable to do so.
Is a DNR the same as a living will?
No, a DNR order and a living will are not the same. A DNR order is a specific medical order not to perform CPR in the event of cardiac or respiratory arrest. A living will, on the other hand, is a broader legal document that outlines a person's preferences for various types of medical treatments and interventions at the end of life, not just CPR. While a living will may include a DNR directive, it also covers other preferences regarding end-of-life care.
Can a Do Not Resuscitate Order be revoked or changed?
Yes, a DNR order can be revoked or changed at any time by the patient or their legally designated decision-maker. To revoke a DNR order, the patient or their representative should inform the attending physician of the decision. The physician will then rescind the DNR order and, if necessary, issue a new medical order based on the patient's updated preferences.
What happens if medical staff are not aware of a patient’s DNR order?
If medical staff are unaware of a patient's DNR order, they may proceed with CPR in the event of a cardiac or respiratory arrest, as it is the standard emergency response. To prevent this, patients with a DNR order are advised to keep a copy of the order with them or ensure it is part of their medical record if they are in a healthcare facility. Additionally, New Jersey residents may also choose to wear a DNR bracelet that alerts medical personnel to their DNR status.
Who should consider a Do Not Resuscitate Order?
Individuals with a terminal illness or those who are in a frail state of health and wish to avoid aggressive medical interventions at the end of life should consider a Do Not Resuscitate Order. It is a personal decision that should be made after thorough discussion with one's healthcare provider and understanding the implications of such an order.
Common mistakes
In the state of New Jersey, completing a Do Not Resuscitate (DNR) Order form is a critical process for those who wish to legally refuse cardiopulmonary resuscitation (CPR) in the event their breathing stops or their heart ceases to beat. Mistakes in completing this form can lead to unintended results, including the administration of life-sustaining treatments that the individual might not want. Below are five common errors made during the completion of the New Jersey DNR Order form:
Not Using the Proper Form: A key mistake is not using the specific form sanctioned by New Jersey for a DNR order. Each state has its own requirements and forms for DNR orders. Using an incorrect form can render the document invalid.
Failing to Include Required Signatures: The New Jersey DNR form requires signatures from both the patient (or their legal healthcare representative) and the physician. Omitting any of these signatures makes the DNR order non-binding.
Incorrect Information: Entering incorrect patient information, such as name, date of birth, or specific medical conditions, can lead to confusion and possible disregard of the DNR order in an emergency situation.
Lack of Witness or Notary Acknowledgment: While some states require a DNR order to be witnessed or notarized, failing to adhere to these specifications, if applicable in New Jersey, may compromise the validity of the document.
Not Communicating with Family Members and Healthcare Providers: A common oversight is not discussing the decision and the existence of the DNR order with family members and healthcare providers. This can lead to confusion and distress during critical moments when the document needs to be presented and acted upon.
Ensuring the accurate completion and proper handling of the DNR form are vital steps in respecting an individual's end-of-life wishes. It is advisable to consult healthcare professionals and legal advisers when completing a DNR order to ensure all requirements are met.
Documents used along the form
When it comes to planning for health emergencies in New Jersey, understanding the key documents that accompany a Do Not Resuscitate (DNR) Order is crucial. A DNR order is just one part of a broader spectrum of advanced care planning. These materials ensure that an individual's medical and personal wishes are respected and followed. The following list provides insight into other forms and documents that are often used alongside a New Jersey DNR Order, each serving a unique purpose in the landscape of healthcare planning.
- Advance Directive for Health Care (Living Will): This legal document lets people state their wishes for end-of-life medical care, in case they become unable to communicate their decisions. It has two parts: the directive itself, where one outlines the care they want or don't want, and the proxy designation, where one names a healthcare representative.
- Medical Power of Attorney (POA): Similar to the second part of an Advance Directive, this standalone document appoints someone to make healthcare decisions on behalf of an individual if they become incapacitated.
- POLST (Practitioner Orders for Life-Sustaining Treatment): This medical order complements a DNR by providing more comprehensive directions about life-sustaining treatments beyond CPR, including intubation, antibiotics, and feeding tubes.
- Last Will and Testament: While not directly related to healthcare, this document specifies how an individual’s property and affairs should be handled after death, and can include funeral wishes and the appointment of an executor.
- HIPAA Authorization Form: This form allows healthcare providers to disclose personal health information to designated individuals, not just those appointed under a Medical POA or a healthcare representative outlined in an Advance Directive.
- Out-of-Hospital DNR: Specifically intended for use outside of hospital settings, this form instructs emergency medical personnel not to perform CPR or other life-saving measures in non-hospital settings.
- Organ and Tissue Donation Registration: An optional form that registers an individual’s decision to donate their organs and tissues upon death.
- Guardianship Designation: This document is pertinent if an individual has specific wishes regarding who should become their guardian in the event they become incapacitated and haven’t appointed a healthcare representative or power of attorney.
- Psychiatric Advance Directive: An important document for individuals with mental illness, specifying their preferences for treatment and care in the event of a mental health crisis where they’re unable to make decisions for themselves.
- Emergency Contact Form: Although not a legal document, having an updated list of emergency contacts readily available for healthcare providers ensures that family members or designated individuals can be reached quickly in an emergency.
Each of these documents plays a vital role in ensuring an individual's healthcare preferences are known, respected, and executed according to their wishes. They collectively provide a comprehensive framework that supports individuals, their families, and their healthcare providers in making informed decisions during critical times. Whether used individually or together, these forms empower individuals to maintain control over their healthcare journey, even in situations when they may not be able to voice their wishes directly.
Similar forms
A Living Will: This document specifies a person's preferences regarding medical treatment if they become incapacitated and cannot communicate their wishes. Like a Do Not Resuscitate Order, it provides clear instructions to medical providers about care preferences.
A Medical Power of Attorney: This designates another individual to make healthcare decisions on a person’s behalf if they're unable to do so. It's similar in its purpose to ensure that medical treatments align with the patient's beliefs and preferences.
A Health Care Proxy: Similar to a Medical Power of Attorney, this document appoints someone to make healthcare decisions for a person when they can't. It ensures decisions are guided by someone who understands the person’s desires.
A POLST Form (Physician Orders for Life-Sustaining Treatment): Much like a Do Not Resuscitate Order, this provides specific instructions about medical care preferences in a clear and direct manner. However, it covers a broader range of treatments beyond resuscitation.
A Durable Power of Attorney for Healthcare: This grants a designated agent the authority to make all health care decisions, not just those about life support or resuscitation, mirroring the comprehensive approach of a Do Not Resuscitate Order in addressing potential healthcare scenarios.
An Advance Directive: This is a broader term that can encompass various types of healthcare directives, including a Living Will and a Do Not Resuscitate Order. It's similar in that it plans ahead for medical care preferences when the person cannot voice them.
A Last Will and Testament: While primarily focused on the distribution of assets and guardianship matters, it's similar in its foresight and preparation for future circumstances, ensuring that personal matters are handled according to the individual's wishes.
A Guardianship Designation: Although its main focus is appointing someone to make decisions on behalf of a minor or an incapacitated adult, its core is the protection and respect for the individual’s preferences and welfare, mirroring the intent behind a Do Not Resuscitate Order.
An Organ Donor Registration: This specifies a person's wish to donate their organs after death. It shares the commonality with a Do Not Resuscitate Order in that it makes personal health care preferences known in advance, affecting posthumous medical decisions.
Dos and Don'ts
Filling out a New Jersey Do Not Resuscitate (DNR) Order requires careful attention to detail and legally-sensitive information handling. Below are crucial dos and don'ts to consider when completing this vital document.
- Do get clear guidance: Involve a healthcare provider in the discussion to fully understand the implications of a DNR order.
- Don't rush through it: Take your time to read and understand each section before filling it out to avoid errors or misunderstandings.
- Do verify patient identity: Ensure the patient's name and other identifying information are accurately recorded to prevent any misapplication of the DNR order.
- Don't overlook witness requirements: Most forms require witness signatures to validate the DNR order. Understand who can or cannot serve as a witness.
- Do discuss with family or healthcare proxy: It's important that family members or a designated healthcare proxy are aware of the patient's wishes concerning resuscitation efforts.
- Don't assume it's immediately effective: Check the requirement for it to be effective. Usually, a physician or authorized healthcare provider must sign the form.
- Do keep the form accessible: After completion, the DNR order should be kept in an easily accessible location, and family members should know where it is.
- Don't use unclear language: If an additional directive is added, make sure the language is clear and unambiguous to avoid potential confusion during critical times.
- Do review and update as necessary: Personal wishes and legal requirements may change. Review the DNR order periodically and update it as needed to reflect current wishes and laws.
Misconceptions
When it comes to the New Jersey Do Not Resuscitate (DNR) Order form, there are several misconceptions that need to be clarified to ensure that individuals and their families can make well-informed decisions regarding end-of-life care. Below are seven common myths and the truths behind them:
- Myth: A DNR Order is only for the elderly.
Truth: A DNR Order can be appropriate for patients of any age who have serious illnesses or conditions that would make CPR not beneficial in the eyes of the patient and their healthcare provider. - Myth: Signing a DNR means you won’t get any medical treatment.
Truth: A DNR Order specifically relates to the omission of CPR if your heart stops or you stop breathing. It does not mean that other treatments, especially those meant to provide comfort, will be stopped. - Myth: You can issue a DNR Order verbally to your healthcare provider.
Truth: In New Jersey, a formal DNR Order must be written and signed by a licensed healthcare provider to be legally valid. Verbal wishes alone are not sufficient. - Myth: All family members must agree for a DNR Order to be implemented.
Truth: While involving family members in these discussions is important, only the patient or their legally designated healthcare proxy can authorize a DNR Order. - Myth: A DNR Order is permanent and cannot be revoked.
Truth: A DNR Order can be revoked at any time by the patient or their designated proxy simply by expressing the wish to do so to healthcare providers. - Myth: Emergency Medical Services (EMS) personnel will not respect a DNR Order.
Truth: If provided with a valid DNR Order or DNR bracelet, EMS personnel are legally required to respect the patient's wishes as outlined in the Order. - Myth: A DNR Order applies to all hospital situations.
Truth: A DNR Order is specific to the use of CPR in situations where breathing stops or the heart stops beating. It does not apply to other medical interventions and treatments.
Understanding the facts about the New Jersey DNR Order can help ensure that your healthcare wishes are respected and that you receive the type of care that aligns with your preferences and values. Always discuss your wishes and any potential orders with healthcare providers to make sure they are clearly understood and appropriately documented.
Key takeaways
When dealing with the New Jersey Do Not Resuscitate (DNR) Order form, understanding its purpose and correctly filling it out is crucial. Here are ten key takeaways to keep in mind:
The DNR form is specifically designed for individuals who do not wish to have cardiopulmonary resuscitation (CPR) in the event their heart stops beating or they stop breathing. This is a critical decision that should be made after thorough discussion with healthcare providers and family members.
It must be completed and signed by a licensed physician, advanced practice nurse, or physician assistant. This endorsement confirms that the healthcare professional has discussed the implications of the DNR order with the patient (or the patient's legal representative).
The form requires clear identification of the patient, including their full name, date of birth, and other relevant personal information, ensuring there is no confusion about the patient's identity.
Patient autonomy is a priority; therefore, the patient’s signature (or that of their legal healthcare representative, if the patient is unable) is necessary to validate the form. This ensures that the decision is made by or on behalf of the patient willingly and without coercion.
The DNR order should be reviewed periodically, especially if the patient's health status changes. This is because decisions regarding life-sustaining treatments can evolve over time based on new information or changes in personal preferences.
A copy of the DNR order should be readily accessible. It is advisable to have multiple copies: one at home, one with a close family member or friend, and one in the medical records with any healthcare providers.
Emergency Medical Services (EMS) personnel are trained to look for a DNR order. Presenting the document promptly in emergencies can ensure that the patient’s wishes are respected.
It's important to communicate your wishes regarding the DNR order with your family members and healthcare proxy. This can alleviate potential distress or confusion during emergency situations.
The legal validity of the form is specific to New Jersey. If traveling or moving out of state, check the requirements and transferability of your DNR order with the relevant state health departments or consult a healthcare attorney.
Completing a DNR form is a decision that can be revised. If a patient changes their mind, it is crucial to inform all relevant parties, revoke the current DNR order, and if desired, replace it with a new one reflecting the current wishes.
Remember, the DNR form is a legal document that requires careful consideration and clear communication. It serves as an expression of a patient's wishes regarding end-of-life care, making it a significant part of healthcare planning.
Create Other Do Not Resuscitate Order Forms for US States
Dnr Do Not Resuscitate - Pre-arranged instructions intended to communicate a patient’s desire to avoid emergency interventions such as CPR.
Dnr Order - By stipulating not to use CPR, it directs medical staff to provide comfort care instead of trying to extend life.
Dnr Oklahoma - A vital healthcare document that clearly states a patient's wish not to undergo resuscitation in the event they stop breathing or their heart stops.
Ct Dnr Form - Healthcare proxies or powers of attorney can also play a role in ensuring a patient's DNR wishes are followed, especially if the patient is unable to communicate.