Blank Do Not Resuscitate Order Form for Texas
In the state of Texas, a pivotal document exists for individuals wishing to express their preferences regarding life-sustaining treatments in the event they are unable to communicate their wishes. Known as the Texas Do Not Resuscitate (DNR) Order form, this legal document plays a crucial role in healthcare and end-of-life planning. It is aimed at informing medical professionals about a person's desire not to receive certain forms of life-sustaining treatment, particularly cardiopulmonary resuscitation (CPR), in cases where their heart stops beating or they stop breathing. The release and management of this form involve a careful process that is designed to respect the patient's autonomy while ensuring that healthcare providers are clear on the patient’s medical treatment preferences. This form, thus, stands as a significant piece of medical documentation, highlighting the importance of individual choice in medical care, and the complexities involved in its execution and adherence by healthcare professionals. It underscores the balance between patient rights and the medical ethics guiding the provision of healthcare.
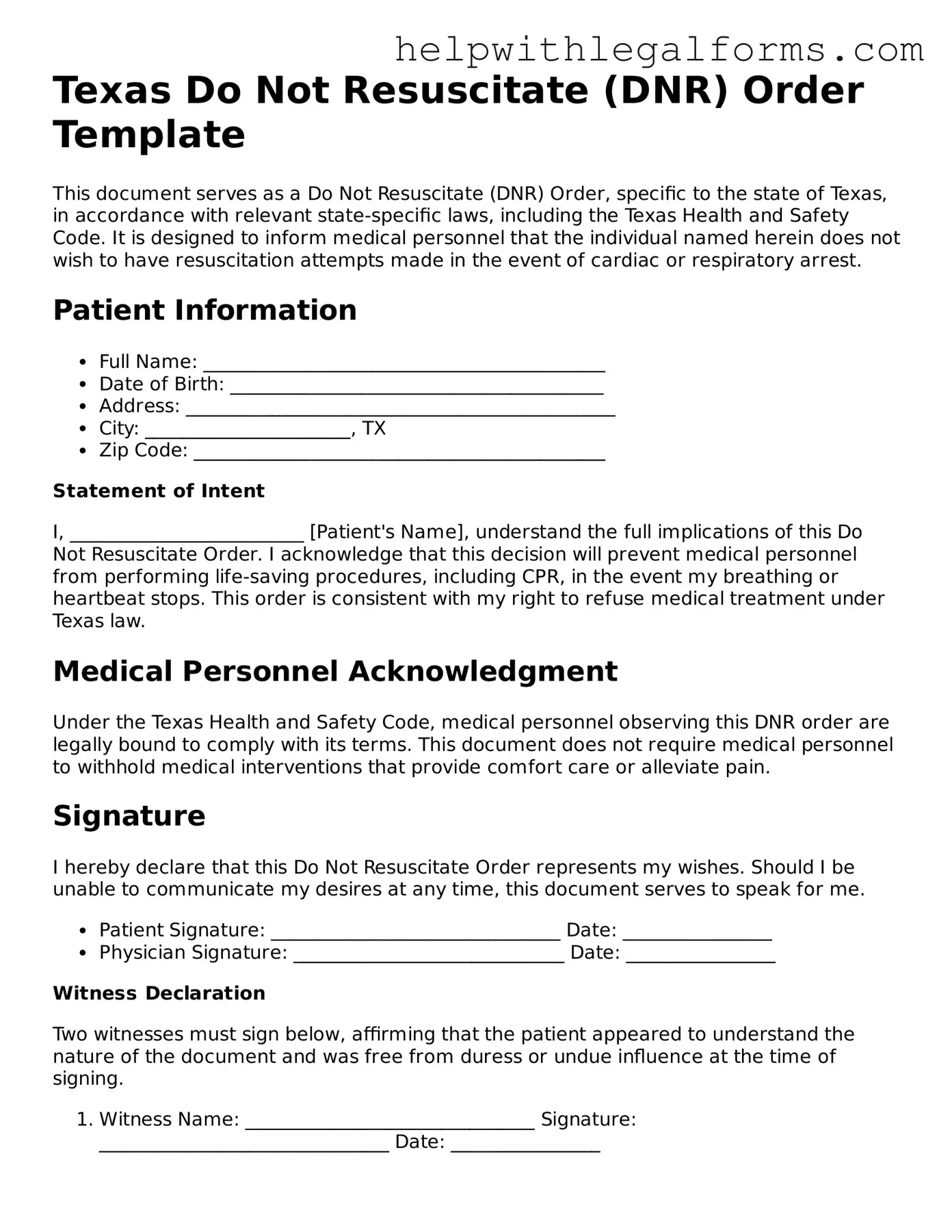
Example - Texas Do Not Resuscitate Order Form
Texas Do Not Resuscitate (DNR) Order Template
This document serves as a Do Not Resuscitate (DNR) Order, specific to the state of Texas, in accordance with relevant state-specific laws, including the Texas Health and Safety Code. It is designed to inform medical personnel that the individual named herein does not wish to have resuscitation attempts made in the event of cardiac or respiratory arrest.
Patient Information
- Full Name: ___________________________________________
- Date of Birth: ________________________________________
- Address: ______________________________________________
- City: ______________________, TX
- Zip Code: ____________________________________________
Statement of Intent
I, _________________________ [Patient's Name], understand the full implications of this Do Not Resuscitate Order. I acknowledge that this decision will prevent medical personnel from performing life-saving procedures, including CPR, in the event my breathing or heartbeat stops. This order is consistent with my right to refuse medical treatment under Texas law.
Medical Personnel Acknowledgment
Under the Texas Health and Safety Code, medical personnel observing this DNR order are legally bound to comply with its terms. This document does not require medical personnel to withhold medical interventions that provide comfort care or alleviate pain.
Signature
I hereby declare that this Do Not Resuscitate Order represents my wishes. Should I be unable to communicate my desires at any time, this document serves to speak for me.
- Patient Signature: _______________________________ Date: ________________
- Physician Signature: _____________________________ Date: ________________
Witness Declaration
Two witnesses must sign below, affirming that the patient appeared to understand the nature of the document and was free from duress or undue influence at the time of signing.
- Witness Name: _______________________________ Signature: _______________________________ Date: ________________
- Witness Name: _______________________________ Signature: _______________________________ Date: ________________
PDF Form Attributes
| Fact | Description |
|---|---|
| Purpose | A Texas Do Not Resuscitate (DNR) Order form is used to inform medical professionals not to perform cardiopulmonary resuscitation (CPR) in the event an individual’s breathing stops or if the individual’s heart stops beating. |
| Governing Law | The form is governed by the Texas Health and Safety Code, Chapter 166.002. |
| Eligibility | To have a DNR order in Texas, the individual must be 18 years of age or older, or if under 18, their parent or legal guardian can request the order. |
| Form Requirement | For a DNR order to be valid, it must be in writing, signed by the individual or their legally authorized representative, and a physician. |
| Revocation | An individual or their authorized representative can revoke the DNR order at any time by any means of communication. |
| Scope | The DNR order applies to CPR only and does not affect other treatments or medications meant to provide comfort care or alleviate pain. |
| Form Validity Out-of-State | A Texas DNR order may not be recognized in other states due to varying laws and requirements. |
| Hospital Policies | Hospitals in Texas may have their own policies regarding the implementation of DNR orders, but they must comply with state law. |
| Emergency Medical Services (EMS) | EMS personnel are obliged to follow DNR orders if presented with the document upon arrival. |
Instructions on How to Fill Out Texas Do Not Resuscitate Order
A Texas Do Not Resuscitate (DNR) Order is a legal document that informs medical professionals not to perform cardiopulmonary resuscitation (CPR) if a patient's heart stops or if they stop breathing. This form is crucial for individuals who want to avoid aggressive life-saving measures due to various personal or medical reasons. Properly completing the DNR form ensures that a person’s wishes regarding end-of-life care are respected and followed. Below are the steps required to fill out this form, ensuring clarity and adherence to legal standards.
- Download the official Texas Do Not Resuscitate Order form from the Texas Department of State Health Services website or obtain a copy from your healthcare provider.
- Read the form thoroughly to understand the implications and requirements. It's important to be fully aware of what the DNR order entails before proceeding.
- Fill in the patient's full name, date of birth, and address in the designated areas to ensure proper identification.
- Discuss the decision with a healthcare provider. The form requires the signature of a physician, advanced practice registered nurse (APRN), or physician assistant (PA) who is familiar with the patient’s medical condition. This conversation should cover the patient's current health status and the implications of a DNR order.
- Ensure that the attending physician, APRN, or PA signs and dates the form. Their certification confirms that they have discussed the DNR order with the patient (or the patient's legally authorized representative) and that the patient has given informed consent.
- If the patient is able to provide consent, the patient or their legally authorized representative should sign and date the form, indicating their agreement to the DNR order.
- Keep the completed form in an easily accessible location. Copies of the form should be provided to family members, caregivers, and the patient’s healthcare providers to ensure that the DNR order is respected in an emergency.
- Inform close family members or caregivers about the DNR order, where the form is stored, and the reasons for the decision. Communication ensures that everyone involved in the patient's care understands their wishes.
Completing a Texas Do Not Resuscitate Order form involves detailed steps, all of which contribute to ensuring that a person's healthcare preferences are clearly communicated and respected. This process, while emotionally and possibly physically challenging, is an important aspect of medical and end-of-life planning. It requires thoughtful discussions with healthcare providers and loved ones to make educated decisions that align with the patient's values and wishes.
Crucial Points on This Form
What is a Do Not Resuscitate Order (DNR) in Texas?
A Do Not Resuscitate Order (DNR) in Texas is a legal document that tells health care providers not to perform CPR (cardiopulmonary resuscitation) if a person's heart stops beating or if they stop breathing. It's for people who, due to their health condition, want to avoid aggressive life-saving techniques.
How can someone get a DNR order in Texas?
Getting a DNR order in Texas involves consulting with a healthcare provider. The discussion should include the patient's medical condition, the likely outcome of CPR, and the patient's wishes. If a DNR order aligns with the patient's care preferences, the healthcare provider will prepare the necessary paperwork, which must be signed by both the provider and the patient or the patient's legally authorized representative.
Who can consent to a DNR order on behalf of a patient?
If a patient is unable to make their own healthcare decisions, an authorized legal representative, such as a medical power of attorney, legally appointed guardian, or close family member in the absence of the aforementioned, can consent to a DNR order on behalf of the patient.
Where is a DNR order valid?
A DNR order in Texas is valid in any healthcare setting, including hospitals, nursing homes, and in the patient's home. It is also recognized by emergency medical services (EMS), meaning if EMS is called, they will adhere to the order's instructions.
Can a DNR order be revoked or changed?
Yes, a DNR order can be revoked or changed at any time by the patient if they are competent to make their own healthcare decisions, or by the patient's authorized legal representative. To revoke a DNR, it's important to inform all healthcare providers involved in the patient's care and, if applicable, remove the DNR bracelet, if one has been issued.
Is a DNR order the same as a living will?
No, a DNR order is not the same as a living will. A DNR specifically addresses the use of CPR in emergency situations. A living will, on the other hand, is a broader document that outlines a person's wishes regarding various life-prolonging medical treatments in the event they become unable to communicate their decisions due to illness or incapacity.
Common mistakes
Filling out a Texas Do Not Resuscitate (DNR) Order form is a significant step for individuals and their families. It communicates crucial medical care decisions, specifically the wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. However, completing this form accurately is paramount; mistakes can lead to misunderstandings or the non-fulfillment of the individual's wishes. Here are six common errors to avoid:
Not verifying the patient's identity: Ensuring that the patient's full name, date of birth, and other identifying information are correctly filled out is critical. Mistakes in this area can lead to confusion and potentially the misapplication of the DNR Order to the wrong individual.
Incomplete information: Every field in the DNR Order should be completed. Leaving sections blank can lead to ambiguities regarding the person's wishes, especially in critical moments when decisions need to be made quickly.
Failure to have the form signed by the required parties: A Texas DNR Order must be signed by the patient (if competent) or their legally authorized representative, as well as the attending physician. Missing signatures can invalidate the document, rendering it ineffective.
Not using the most current form: Laws and regulations change, and so do the forms that reflect those laws. Using an outdated version may mean that the DNR Order will not be recognized or acted upon as intended.
Lack of witnesses or notary: While Texas law may not require a witness or notary for a DNR Order, having the document witnessed or notarized can add a layer of verification and legality, particularly if the document’s validity is ever questioned.
Not communicating with the family or healthcare proxy: It's essential to discuss the decision to have a DNR Order with family members or a healthcare proxy to ensure that they understand the individual's wishes. Failure to communicate can lead to confusion or distress during emergencies.
Correctly completing a DNR Order helps ensure that an individual's healthcare preferences are respected. Avoiding these mistakes can significantly impact the effectiveness and applicability of the document, ensuring that one's final wishes are honored and that families are spared unnecessary stress during difficult times.
Documents used along the form
In the state of Texas, alongside a Do Not Resuscitate (DNR) Order form, several other important legal documents are frequently utilized to ensure an individual's healthcare wishes are well-documented and respected. These documents complement each other to provide a comprehensive approach to end-of-life care planning. Understanding each document's purpose and scope can significantly aid individuals and families in making informed decisions about healthcare planning.
- Medical Power of Attorney: This document allows an individual to appoint another person (known as an agent) to make healthcare decisions on their behalf if they become incapable of making their decisions. It is different from a DNR because it covers a wide range of decisions beyond resuscitation.
- Advance Directives: Often referred to as a living will, this document allows individuals to outline their wishes about medical treatment and life-sustaining measures if they become terminally ill or incapacitated and cannot communicate their healthcare preferences.
- Out-of-Hospital Do Not Resuscitate Order: Specifically designed for situations occurring outside of hospital settings, this document instructs emergency medical personnel not to initiate CPR or other life-sustaining treatments. It supports the individual's wishes concerning resuscitation in non-hospital environments.
- Physician Orders for Scope of Treatment (POST): This is a physician's order that outlines a plan of care respecting the patient's wishes concerning treatment at the end of life. It is designed for patients with serious illnesses and specifies which treatments should be applied or not, including resuscitation.
The interplay between these documents can help ensure a well-rounded and person-centered approach to healthcare decision-making. By familiarizing themselves with these documents, individuals can better prepare for the complexities of healthcare needs as they arise, thereby ensuring their medical wishes are respected and adhered to by family members and healthcare providers alike.
Similar forms
Living Will: A Living Will is similar to a Do Not Resuscitate (DNR) Order in that it allows individuals to outline their preferences for medical treatment should they become unable to communicate their wishes. Both documents are proactive measures to ensure that medical treatment aligns with the individual’s values and wishes regarding life-sustaining procedures.
Healthcare Power of Attorney: This document, like a DNR Order, is used to direct medical decisions when an individual is incapacitated. While a DNR specifically addresses the use of measures to restart the heart or breathing, a Healthcare Power of Attorney is broader, allowing a designated agent to make a wide range of health care decisions on behalf of the individual.
Advanced Directive: An Advanced Directive is an umbrella term that can include both Living Wills and DNR Orders. It entails instructions about future medical care. A person can use an Advanced Directive to specify what actions should be taken for their health if they are no longer able to make decisions because of illness or incapacity, much like how a DNR order specifies wishes regarding resuscitation.
Medical Orders for Life-Sustaining Treatment (MOLST): Similar to a DNR, MOLST forms detail what types of life-sustaining treatment a person wants or doesn't want, including CPR. These forms are intended for people with serious health conditions and provide instructions that are immediately actionable by healthcare providers.
Five Wishes Document: Often considered a combination of a Living Will and a Healthcare Power of Attorney, the Five Wishes Document goes beyond traditional medical and legal language to address personal, emotional, and spiritual needs alongside medical wishes, including circumstances under which one would not want to be resuscitated.
Physician Orders for Scope of Treatment (POST): Similar to a DNR, a POST form is designed for individuals with serious illness or frailty towards the end of life. It translates the individual’s wishes about certain medical treatments, including resuscitation, into medical orders.
Durable Power of Attorney for Healthcare: This is similar to a Healthcare Power of Attorney and complements a DNR by allowing an individual to appoint someone to make health care decisions on their behalf. It remains effective even if the person becomes incapacitated, ensuring that their medical treatment preferences are respected and followed.
Emergency Medical Services (EMS) DNR Order: Specifically designed for emergency medical services, an EMS DNR informs emergency personnel not to perform CPR. Similar to a hospital-issued DNR, this document is used when an individual wishes to avoid resuscitation attempts in the event of cardiac or respiratory arrest outside of a hospital setting.
Dos and Don'ts
Filling out a Texas Do Not Resuscitate (DNR) Order requires careful attention to detail and an understanding of its implications. The DNR order communicates a patient's wish not to have cardiopulmonary resuscitation (CPR) in the event their heart stops or they stop breathing. Below are essential dos and don'ts to guide you through the process:
Do:- Read the instructions carefully before filling out the form to ensure you understand all the requirements and implications of a DNR order.
- Ensure all information is accurate and complete, including the patient's full name, date of birth, and the specific medical conditions leading to the request for a DNR.
- Discuss the decision with family members or a healthcare proxy to ensure that your wishes are understood and will be respected.
- Consult with a healthcare provider to understand the medical implications and ensure that the DNR order is appropriate for your situation.
- Sign and date the form in the presence of the required witnesses or a notary public, as specified by Texas law.
- Keep the original document in a safe but accessible place and provide copies to your family, healthcare proxy, and primary care physician.
- Fill out the form without fully understanding the conditions under which the DNR order will and will not apply.
- Forget to update the DNR order if your health condition or wishes change. A new form should be completed to reflect any changes.
- Assume all healthcare providers automatically know about your DNR order. Make sure to communicate your wishes to all involved in your care.
- Fill the form out in haste without discussing it with a trusted healthcare provider or understanding the full legal implications.
- Neglect to inform close family members or caregivers of your decision, as they may be involved in critical discussions during an emergency.
- Leave the DNR order where it cannot be easily found. Ensure that it is readily accessible in an emergency situation.
Misconceptions
When discussing the Texas Do Not Resuscitate (DNR) Order form, there are several misconceptions that often cloud understanding. It's crucial to dispel these myths to ensure individuals make informed decisions about their end-of-life care wishes. Here are six common misunderstandings:
- Myth 1: A DNR affects all medical treatments. Many believe that a DNR order limits all forms of medical treatment. However, it specifically applies to the avoidance of CPR (cardiopulmonary resuscitation) in the event of cardiac or respiratory arrest. It does not hinder other treatments, including pain management, antibiotics, or nutrition.
- Myth 2: Only the elderly or terminally ill can opt for a DNR. This isn't true. While it's common among these groups, a DNR is available to anyone who wishes not to have CPR performed if their heart stops or they stop breathing. This decision can be based on various personal reasons and medical conditions.
- Myth 3: A DNR is irreversible. People often think once a DNR order is signed, it cannot be changed or revoked. That's not the case. A DNR order can be revoked at any time by the individual or their legally authorized representative, ensuring that choices about end-of-life care remain flexible.
- Myth 4: Verbal DNR orders are legally binding in Texas. Verbal DNR orders, although respected in emergency situations by healthcare providers, are not legally binding in Texas. For a DNR order to be legally recognized, it must be documented on the Texas DNR order form, signed, and in accordance with Texas law.
- Myth 5: A DNR order is only valid in a hospital setting. In Texas, a DNR order is valid in all settings. This means it is effective not just in hospitals, but also in homes, nursing facilities, and during transport by emergency medical services (EMS), ensuring that an individual's wishes are honored everywhere.
- Myth 6: The family can override a DNR. A frequent misconception is that family members or next of kin can override a patient's DNR order. In Texas, a validly executed DNR order reflects the individual's wishes and is legally binding. Family wishes, while important, cannot override a DNR if it contradicts the patient’s explicit instructions.
Understanding the Texas DNR Order form is crucial for ensuring individuals' rights and wishes are respected at the end of life. Dispelling these myths fosters better communication between patients, families, and healthcare providers, leading to more informed and respectful decision-making processes.
Key takeaways
Filling out and using the Texas Do Not Resuscitate (DNR) Order form involves several key considerations for individuals, their families, and healthcare providers. Below are nine essential takeaways that are important to understand:
- Clear Intent: The Texas DNR Order form is designed to communicate a person's wish not to receive cardiopulmonary resuscitation (CPR) in the event that their breathing stops or their heart stops beating.
- Form Requirement: For the DNR order to be valid, it must be filled out correctly and comply with Texas state requirements. This includes the signature of the individual (or their legally authorized representative) and the physician.
- Physician's Role: A physician must agree that the DNR is in the best interest of the person's health, taking into account their medical condition and wishes. The physician's signature is essential for the order's validity.
- Revocation Process: Individuals have the right to revoke their DNR order at any time. This revocation can be done verbally or in writing, and it is imperative to communicate this revocation to the healthcare provider immediately.
- Storage and Accessibility: Once signed and completed, the DNR order should be stored in a place where it can be easily accessed by family members or caregivers, and presented to healthcare providers when necessary.
- Portability: The Texas DNR order is recognized across different healthcare settings within the state, including hospitals, nursing homes, and in-home care. It is important to ensure that the order follows the individual wherever they receive care.
- Legality: The Texas DNR order is a legal document under state law. It must be respected by healthcare professionals, and failing to do so can have legal implications.
- Communication is Key: Discussing the decision to have a DNR order with family members and healthcare providers is crucial. It ensures that everyone involved understands the individual's wishes and the reasons behind them.
- Review and Update: As circumstances change, it is advisable to review the DNR order periodically. Changes in health status or personal wishes may necessitate updating or revoking the order to ensure it reflects the person's current desires.
Create Other Do Not Resuscitate Order Forms for US States
Dnr Do Not Resuscitate - An expression of patient autonomy, outlining their decision against the use of life-saving measures in dire circumstances.
Ct Dnr Form - Emergency medical services (EMS) and hospital staff are trained to look for these orders in situations where immediate decisions are required.
Dnr Order - Often used by patients with chronic conditions, ensuring they avoid the cycle of emergency interventions.
How to Get a Do Not Resuscitate - Guides healthcare professionals in respecting a patient's wishes by clearly stating the refusal of life-preserving actions through resuscitation.